Swiss ICU capacity during Covid19
Switzerland has justified lockdowns and the Covid-Zertifikat by the danger of its hospital ICU beds running out — while removing beds and overestimating the impact of Covid19 by up to 2x.
In Switzerland, a large motivator behind the lockdowns of 2020, and the subsequent introduction of the Covid-Zertifikat in 2021, has been the availability of Intensive Care Units (ICU) hospital beds. These beds, locally called Intensivbetten, have the equipment necessary to treat serious cases of Covid19.
Reading the mainstream news, one gets the impression that the beds are in immediate danger of running out unless strict measures are enacted (de). Indeed, the recent federal restrictions, locally called the 3G rules, were justified by an increasing percentage of all ICU beds being occupied by Covid19 patients.
The 3G rules prohibit residents from going to restaurants, dance classes, yoga, and in some cases even working unless they accept regular testing (Getestet) or vaccination (Geimpft). The third G, Genesen, stands for recovered. It requires a positive PCR test taken within the last six months. Tests indicating antibodies or T-cells are not sufficient, even though natural immunity is superior and protects longer than vaccination.
In this article we will first focus on the ICU capacity of Switzerland, how it has been decreasing for ten years and how it compares to other European countries. Next, we will look into the accuracy of the Covid19 ICU bed occupancy, and develop a model which allows us to estimate the true ICU impact of Covid19.
The decreasing ICU capacity
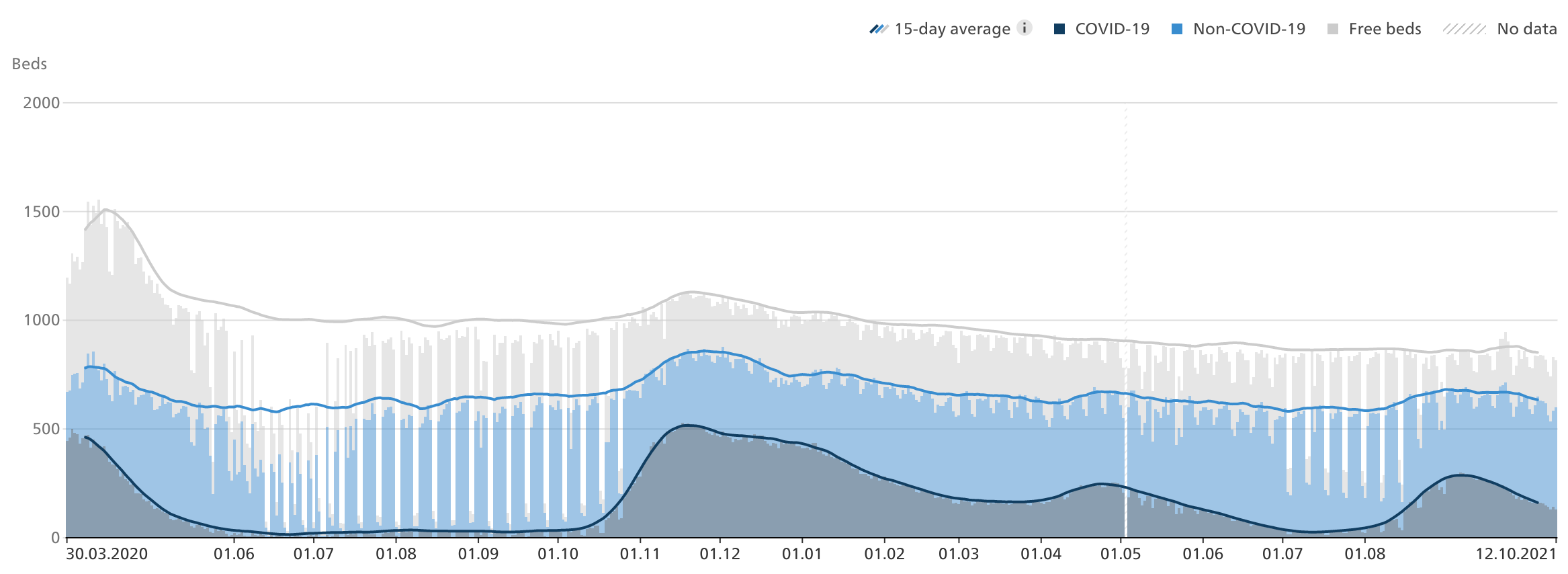
The Swiss Federal Office of Public Health publishes detailed statistics of the occupancy and availability of ICU beds. Let us look at an overview:
The number of ICU beds has been consistently decreasing from a peak at around 1500 during the first Covid19-wave in 2020, to just about 850 today.
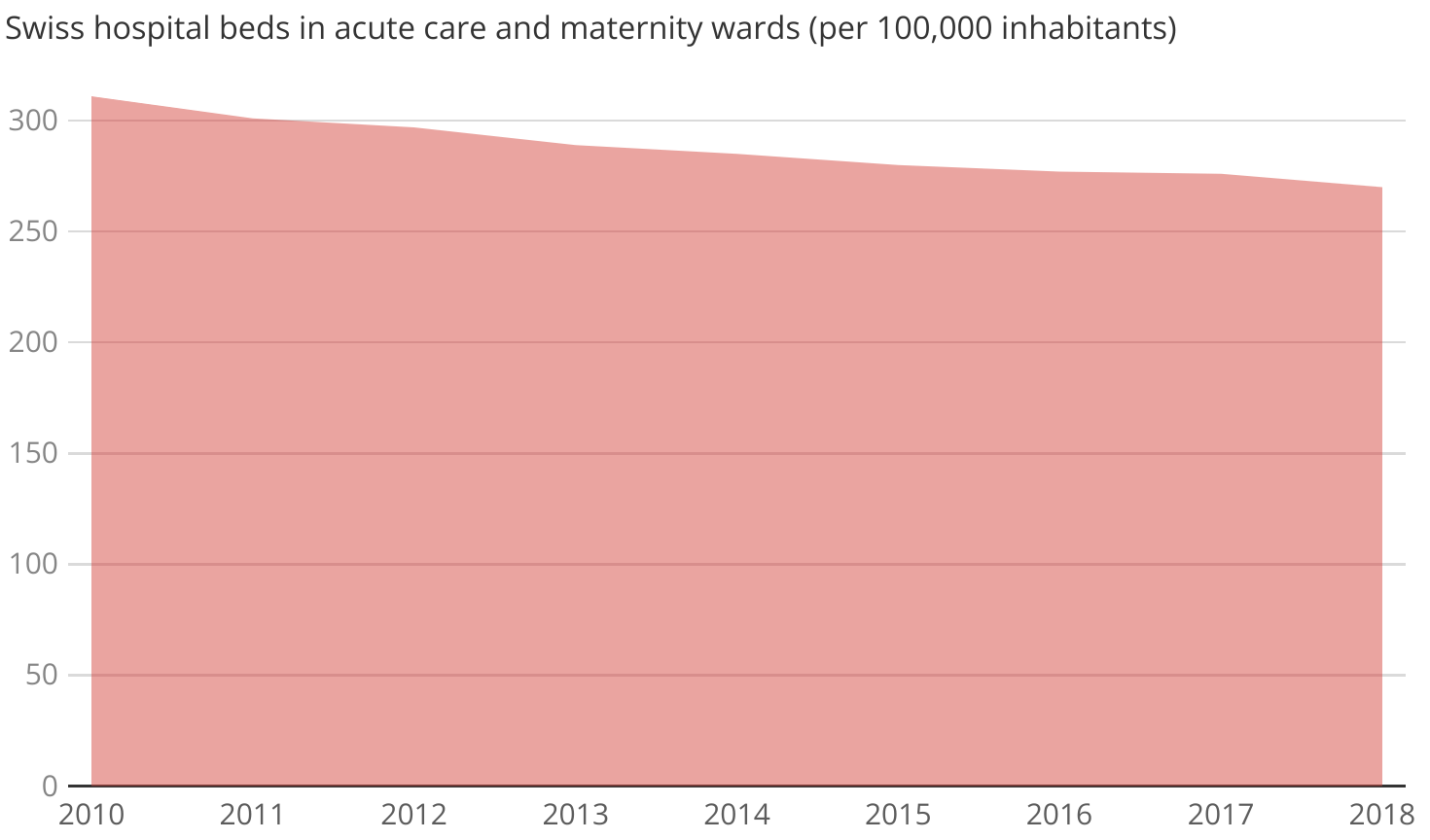
We only have detailed statistics of ICU beds starting from the beginning of the Covid19 pandemic. However, we do have numbers showing us that the number of hospital beds, in general, has trended downwards since at least 2010:
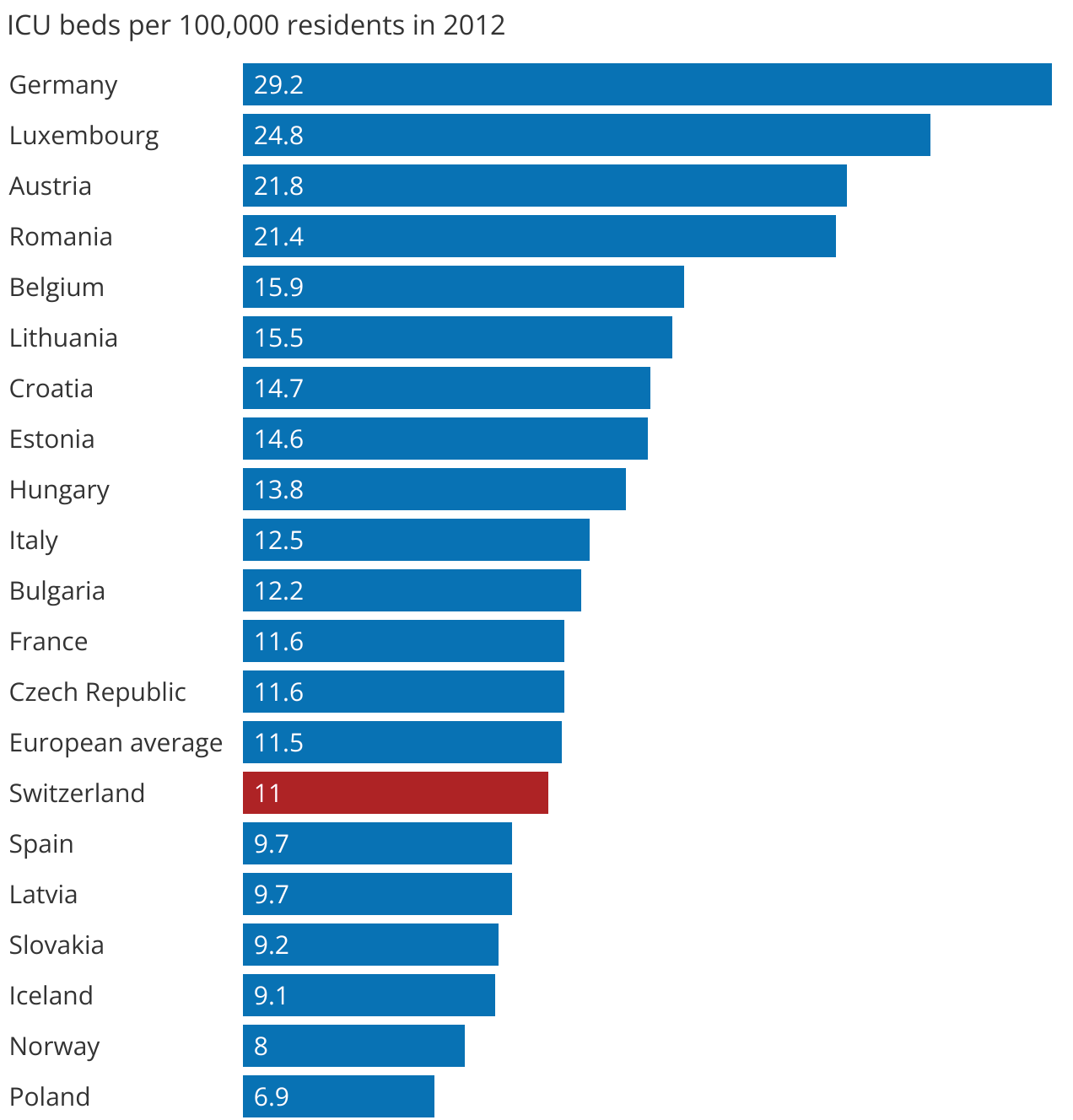
Statistics regarding the average number of ICU beds in Switzerland and other European countries are available for 2012. Switzerland, with its 11.0 ICU beds per 100'000 residents — is far from its cultural and geographical neighbors Germany and Austria who have 2-3 times the capacity, with 29.2 and 21.8 ICU beds respectively. Switzerland's capacity is instead similar to countries like Spain, Latvia and the Czech Republic.
Why did the capacity decrease until the first wave in 2020? A reasonable hypothesis is cost-cutting. It's tempting to save money and remove capacity that have not been used for a long time.
The second and more important question is why do the hospital beds continue to decrease since the start of the pandemic. Swissinfo, a publicly financed news channel, argues that it's due to lack of educated nursing staff (de). Le News argues fatigue and exhaustion due to the lack of personnel. While ICU equipment is easy to buy, hospital workers require time to educate.
If we assume that the under-capacity of ICU beds was the primary reason behind the measures, we can estimate how much it cost Switzerland by looking at its economy. While it's impossible to answer “but what if” scenarios, very coarse approximations still provide some insight. Let us compare with Sweden, another European country with a highly developed economy and advanced workforce. Sweden, in stark contrast to most countries, didn't lock down its society and economy. Let us compare the Gross Domestic Product (GDP) of Switzerland vs. Sweden for 2020.
| GDP 2020 | Growth | |
|---|---|---|
| Sweden | 4'951'559 million SEK | -1.3% |
| Switzerland | 706'242 million CHF | -2.4% |
Switzerland's GDP shrunk almost twice the amount that of Sweden. Let us assume, that without harsh measurements, the GDP growth of Switzerland would've been the same as Sweden's — recovering 1.1 percentage points of the decrease. That's 7'272 million additional CHF. Let us assume that Switzerland had added an additional 33% ICU beds at the peak of the first wave in March 2020. An extra 500 new beds with each bed costing up to 14.5 million CHF to operate per year would still have been a better decision, with a net economic advantage over the implemented measures.
The economic reality is more complex than our analysis. GDP does not capture all economic aspects, and we cannot assume Switzerland's GDP would have behaved the same way as Sweden's. One could write a PhD thesis analyzing the economic impact of various measures. A very coarse analysis does give us a hint of the magnitude of the cost. Had the lockdowns only been responsible for 0.11 percentage points of the decrease, it would still leave us with 1.45 million CHF per additional ICU bed per year.
ICU beds may be expensive, but it is more expensive to lock down a society. It would be sound to increase the number of ICU beds for the future. Covid19 is not the first pandemic, and it won't be the last.
Sources:
- Swissinfo: Swiss economy suffers worst slump in 45 years.
- Statista: Sweden Gross domestic product.
- Swiss Federal statistics office: Gross Domestic Product
The ICU occupancy paradox
In all the Covid19 waves, the same pattern occurs: When Covid19 ICU occupancy increases, Non-Covid19 occupancy decreases. As there are plenty of free beds at all times a medical triage where non-Covid19 patients are moved to non-ICU beds is unlikely. Where do the non-Covid19 patients go?
The following non-stacked line plot shows the apparent inverse correlation between Covid19 and Non-Covid19 patients clearly:
This is a discrepancy — why do more Covid19 patients lead to less Non-Covid19 patients?
To understand why, we will first look into the accuracy of determining the Covid19 diagnosis, the PCR test. After that, we will present a statistical model that allows us to estimate the true extra impact of Covid19 on the ICU beds in Switzerland.
Unreliable PCR tests
Covid19 cases are verified using the PCR test. The test's accuracy is still not established. Analyzing the accuracy is complicated. It is greatly affected by the time since the onset of the first symptoms and technical details regarding how the test is performed.
Phil M. Bentley, a researcher at the multi-disciplinary European Spallation Source whose previous work include nuclear physics research, has studied the accuracy of the test. The study estimates its accuracy for three classes based on the severity of the symptoms:
- No symptoms.
- Mild symptoms.
- Severe symptoms.
3.4.5 Severe symptoms
This patient from a social pool with 600 cases per 100k population is admitted to hospital complaining of severe symptoms and is immediately given a test. The analysis is shown in Table 7. Before testing, the patient has a 29% probability of being infected. If the test returns a positive result, they have a 62–91% probability of being infected (depending on the false positive rate), and if negative they have a 13–15% probability of being infected.
– Error rates in SARS-CoV-2 testing examined with Bayes' theorem
The study suggests that between 9%–38% of all patients with severe respiratory illness symptoms and a positive Covid19 PCR result do not have Covid19. For mild and no cases the accuracy is even worse: only 0.6%–4% of all asymptomatic people with a positive test have Covid19. For mild symptoms, the percentage is 10%–42%. The estimated numbers cast a shadow of uncertainty over the official infection statistics.
A model for excess ICU beds
Plotting the Non-Covid19 ICU patients as a function of Covid19 patients reveals a surprisingly clear negative linear correlation. For each patient that tested positive for Covid19, 0.48 Non-Covid patients disappeared from the intensive care unit. The correlation is far too strong to happen by chance. It indicates that up to 48% of patients classified as Covid19-positive may have occupied ICU beds regardless. The number is significantly worse than the upper bound inaccuracy estimation of the PCR-test by Phil M. Bentley.
We must be careful to not immediately conclude that the PCR test is responsible for the entire discrepancy. Another co-factor could for example be that a percentage of Covid19-positive patients would have ended up in the ICU regardless. If not from Covid19, then from some other disease.
A third explanation is that some patients' elective surgeries were delayed (de) in anticipation of Covid19 waves. An elective surgery is not a medical emergency but may still require an ICU bed. We have unfortunately not found any quantitative data to support or reject this. While it is possible that it explains part of the discrepancy, we do not think it can explain the entire:
- There are always plenty of free ICU beds available that can absorb the need from elective surgeries. What is the spare capacity for if not to absorb more patients?
- The system shows great flexibility in adding or removing beds in short notice. The actual spare capacity is likely larger than the “free beds” area in the occupancy plot.
- There is no time-delay between the Covid19 and non-Covid19 inverse correlation. If the reduction would be in anticipation of Covid19 waves, the decrease in non-Covid19 would happen before the waves. If it would be a reaction, it would happen after. The data shows a real-time system. It is unlikely that planners for elective surgeries could react that fast and consistently during all waves.
- Germany, with its larger ICU capacity and significant reserve, still demonstrates the same pattern.
If indeed a large part of elective surgeries were cancelled, it would weaken this part of the article, but strengthen the first part. The decade-long decrease of ICU beds would have prevented many patients from receiving their elective surgeries in a timely manner.
To estimate the additional impact of Covid19 on the medical system, we can subtract the cases that may have ended up in the ICU anyway from the Covid19 part and add them to the Non-Covid19 part:
Formula for estimating additional impact
| Covid19' | = | (1 - 0.48) * Covid19 |
| NonCovid19' | = | NonCovid19 + 0.48 * Covid19 |
Adjusted plots
Conclusion
When faced with the uncertainty of a new pandemic, it is understandable that strong precautions are initially enacted. We do not know how many people would need ICU beds without the lockdowns and 3G rules. However, if there has been a real danger of the beds running out, why would the capacity continue to be reduced? The cost of having more ICU beds is minuscule compared to the economic impact of the measures and lockdowns. Furthermore, the data used has overestimated the impact of Covid19 — we estimate that up to half of the cases attributed to Covid19 may have ended up in the ICU regardless.
After almost two years of research and data, it is evident that the ICU bed occupancy justifies neither the lockdowns nor the Covid-Zertifikat. It is true that the percentage of free ICU beds continues to decrease. However, it is not because of a large increase in patients, but rather due to a decade-long trend of removing ICU beds. Shortsightedness and an unwillingness to earnestly analyze the situation have caused Switzerland and its people to suffer economically and perhaps more so socially.
Revisions
November 1, 2021
- The GDP argument was clarified to emphasize that GDP is a very coarse metric. It is not intended to be a proof, but rather a hint of the magnitude of the cost.
- The following statement was removed after a discussion with a Portuguese speaker:
Lisbon Court of Appeal has stated that the PCR test “is unable to determine, beyond reasonable doubt, that a positive result corresponds, in fact, to the infection of a person by the SARS-CoV-2 virus”.
It appeared in a context where the PCR test was reported to be unreliable. However, the Lisbon Court of Appeal stated that its accuracy cannot be established beyond reasonable doubt without knowing the technical parameters used for some particular tests, not PCR tests in general. Court decision (Portuguese). - A reader pointed out that part of the ICU bed discrepancy may be explained due to elective surgeries being cancelled. A discussion about it was added, and some statements made by this article weakened.
Next article